Rx Pad
This 5th Edition of Hyperbaric Medicine Practice, captained by Dr. Harry T. Whelan, is the most robust and monumental information source for undersea and hyperbaric medicine to date. Split into two volumes due to its size and detail, this 5th edition boasts six new chapters. With the help of 70 contributors from all over the world, Hyperbaric Medicine Practice has become the go-to authority for both studying and practicing hyperbaric medicine professionals.
There are many scales that attempt to classify diabetic foot ulcers, but few have been validated and none have demonstarated prognistic reliabilty or accuracy with regard to healing a DFU. Some scales focus on anatomy (depth of ulcer), some include vasular assessment, and others include the presence or absence of infection.
Question: I am interested in adding hyperbaric oxygen therapy to my clinic. What are your recommendations for staff education and management of hyperbaric medicine in my clinic?
Answer: The first step we recommend is that you attend a 40-hour UHMS and NBDHMT approved basic training in hyperbaric medicine course, Introduction to Hyperbaric Medicine. Wound Care Education Partners offers the course many times per year across the U.S., and we could also do onsite training at your facility.
Upcoming course dates and locations can be found at the following link https://www.woundeducationpartners.com/live-courses/upcoming-courses.html
As for management, we recommend that you attend our Business of Wound Care and Hyperbaric Medicine course. This 16-hour CME/CEU course guides you through the administration of operating and managing a profitable wound care/hyperbaric clinic. This course is offered a few times per year at various locations across the U.S.
Find upcoming courses at the following link: https://www.woundeducationpartners.com/live-courses/the-business-of-wound-care-and-hyperbaric-medicine.html
For more information on any of our courses please contact us at
The Undersea and Hyperbaric Medical Society (UHMS) is holding their Annual Scientific Meeting (ASM) on June 9-11 in Las Vegas, NV. The ASM is the place to meet the top industry experts and leaders in the field of the undersea and hyperbaric medicine (and no they didn't pay us to say that!).
Copyright
© Wound Care Education Partners. All Rights Reserved.
A question that we get frequent phone calls about is regarding physician supervision of Hyperbaric Oxygen Therapy (HBO). Here are the answers to some of the most frequently asked questions . . .
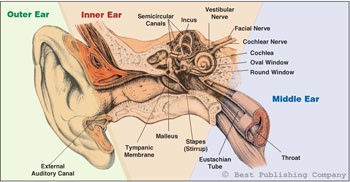
Sinus and internal and external ear disorders are the most common side effects of hyperbaric oxygen therapy (HBO2).1 These spaces are the cranium’s pneumatic sockets and, particularly those of the middle and inner ear, are most frequently involved in the pressure stress caused by compression and decompression maneuvers during exposure to altered pressures in the hyperbaric chamber. Barotrauma is the mechanical tissue damage produced by environmental pressure variation, and the middle ear is the most frequently involved structure in this kind of damage. According to Boyle’s law (the product of pressure and volume is a constant for a given mass of confined gas) it is easy to understand why all enclosed air cavities are more susceptible to this kind of lesion. Barotraumas can occur due to an increase or decrease of gas volume. To avoid gas volume decrease during the compression phase, the patient must perform some compensatory maneuvers aimed at inhaling and forcing gas (air or oxygen) into the nasal and sinus cavities. During decompression in the chamber or even underwater, the body’s gas expands and is expelled from cavities to the outside, usually without any active maneuver. It is essential to teach the patient about the functions of the hyperbaric chamber and the correct maneuvers of baro compensation. In this article, we will describe the main barotraumas that can occur during hyperbaric oxygen therapy.
Copyright
© Wound Care Education Partners. All Rights Reserved.
Copyright
© Wound Care Education Partners. All Rights Reserved.
Many refer to Dr. Eric Kindwall at the "Father of Hyperbaric Medicine," and his contributions to hyperbaric medicine are legendary. Dr. Kindwall was born on January 17, 1934 and passed away on January 18, 2012. For this reason, we find it fitting to highlight his contributions to the field of hyperbaric medicine during the month of January.
Copyright
© Wound Care Education Partners. All Rights Reserved.
We all learn about barotrauma in the Introductory Course in Hyperbaric Medicine. The question we have for you today is whether or not you remember the mechanisms of what causes barotrauma and how to properly pre-screen HBOT patients.
Copyright
© Wound Care Education Partners. All Rights Reserved.
There has been a lot of communication in the marketplace, as well as confusion and misunderstanding, over the past few weeks regarding the final publication details and implementation notice of the Medicare Administrator Contractor’s, Novitas LCD on hyperbaric medicine for hospitals and physicians. The LCD takes effect July 24th, 2014. A major development with MAC’s and commercial insurance products recently, is their taking a stance on practice requirements. They are dictating credentialing standards. This most recent LCD from Novitas reflects that positioning as well. In this blog post we give you straight answers that will provide clarity and assist you in understanding how the revised requirements will impact you and your program staff.
Copyright
© Wound Care Education Partners. All Rights Reserved.
Is it a goal of your clinic to achieve 100% staff credentialing? If not, your facility is missing a huge opportunity. Having a fully credentialed staff sends the message to referring physicians, patients, and your local community that meeting a national standard of high quality health care is your clinic's #1 priority. Being fully credentialed also sends the message that your clinic has a very competent clinical team. And when faced with making a patient referral, wouldn't you rather refer a patient to a facility that you trust to be competent and provide the highest quality of care?
Copyright
© Wound Care Education Partners. All Rights Reserved.
We recently recieved this question from a prospective student. If you find yourself asking this same question, read on to learn the course of action we recommend.
Copyright
© Wound Care Education Partners. All Rights Reserved.
The development of a comprehensive maintenance program for a hyperbaric system and its supporting equipment is essential for a safe and cost-effective operation. The chamber and its operational systems, the chamber room, and the equipment used in and around the chamber should be maintained at the highest operational level. This should also include the cleanliness of all elements of the interior and exterior systems.
Copyright
© Wound Care Education Partners. All Rights Reserved.
Copyright
© Wound Care Education Partners. All Rights Reserved.
Question: "I would be interested in the current perspective regarding supervision of hyperbaric dives by Nurse Practitioners.
Copyright
© Wound Care Education Partners. All Rights Reserved.
Cardiac arrest is a rarity in the chamber, as most arrhythmias seem to improve under hyperbaric conditions. Anecdotally, it can be noted that one patient with a myocardial infarction, who was being treated with hyperbaric oxygen as part of a research study, suffered 30 cardiac arrests during the 48 hours he was being treated with the chamber. The schedule being followed called for two hours at pressure in the chamber followed by one hour on the surface. This cycle was repeated for two days. It can be seen that the patient spent only 1/3 of his time breathing air on the surface. During the study, the patient suffered 28 cardiac arrests while breathing air on the surface, but only two arrests while at pressure in the chamber. The patient eventually recovered and returned to work. (Thurston, J. Westminster Hosp, London, Personal Communication, 1973.)
Copyright
© Wound Care Education Partners. All Rights Reserved.
The cardiovascular assessment of a critical care patient receiving hyperbaric oxygen therapy is similar to any cardiovascular assessment of a critical care patient. Cardiac rhythm should be assessed and monitored during the treatment. If the patient would experience a cardiac emergency during HBO treatment, the staff should be trained to handle such an emergency. It is important to remember that a patient at depth is well oxygenated and will remain so for 5 to 8 minutes. The safest way to bring a patient that has had a cardiac arrest to the surface is to bring them up at 5 psig (fastest rate on a monoplace chamber), while the staff prepares to deliver emergency care. Performing a rapid ascent using the emergency ascent button on monoplace chambers places the person at grave risk for air embolism due to expansion injuries. Once the patient has surfaced, move them to the point farthest away from the open chamber, remove the hyperoxygenated clothing, and if appropriate, defibrillate. Cold oxygen will fall to the floor and dissipate in 30 seconds, so do not place the area at an increased fire risk with the use of a defibrillator. The staff needs to be able to respond quickly and appropriately to such an emergency, so it is our recommendation that the staff be Advanced Cardiac Life Support (ACLS) certified.
Copyright
© Wound Care Education Partners. All Rights Reserved.
Hyperbaric oxygen exposure can produce significant hemodynamic changes. An increase in systemic afterload due to hyperoxic vasoconstriction in well perfused tissues can lead to a decrease in left ventricular function and a decrease in ejection fraction in some patients. When this decrease in left ventricular function occurs in the setting of pulmonary arterial vasodilatation due to improved alveolar oxygenation with increased left atrial and left ventricular filling, acute left ventricular dysfunction and pulmonary edema can result. Cases have been reported in patients with a history of pulmonary edema or low left ventricular ejection fractions or in patients with sudden fluid shifts from volume overload. Acute pulmonary edema appears to be more common in monoplace than multiplace treatment settings, perhaps because of the requirement for patients to be in a more supine position in the monoplace chamber rather than the sitting position with legs dependent available in the multiplace chamber.
Copyright
© Wound Care Education Partners. All Rights Reserved.
Copyright
© Wound Care Education Partners. All Rights Reserved.
Question: Each winter many hyperbaric oxygen therapy patients have difficulty getting to their scheduled treatments due to inclement weather. What recommendations do you have for helping keep patients' treatment schedules on track when the weather is a barrier to treatment?
Copyright
© Wound Care Education Partners. All Rights Reserved.




![[Video] Debridement: Learn How, When, and Why](https://mail.woundeducationpartners.com/images/easyblog_images/176/b2ap3_large_Wound-Care-Review-course-updates_ww.jpg)