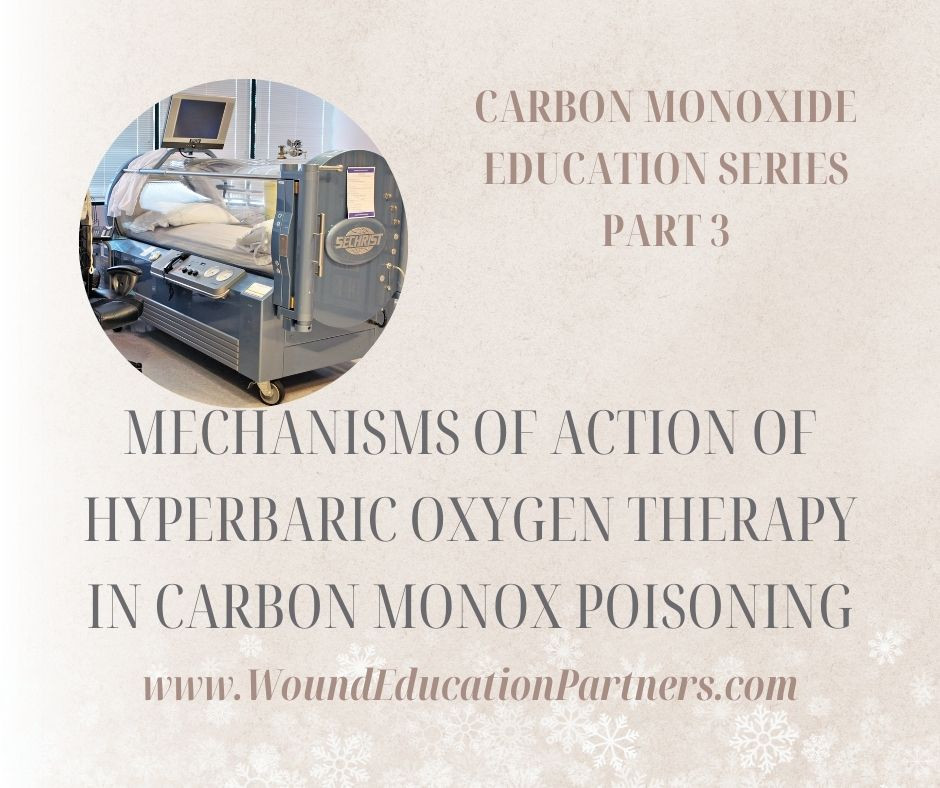
Current knowledge indicates that there are multiple mechanisms of action of hyperbaric oxygen therapy in CO poisoning. Based on the law of mass action, elevated partial pressures of O2 will accelerate the rate of CO dissociation from hemoglobin. Thus, COHb half-life can be decreased from approximately 5 .5 hours when breathing air and to approximately 20 minutes when breathing O2 at 3 ATA. Indeed, this was the reasoning behind the first clinical implementation of hyperbaric oxygen therapy for CO poisoning. As the COHb level is not associated with clinical risk, it is hard to accept that a more rapid dissociation of CO from hemoglobin could be the central factor for the benefit of hyperbaric oxygen . A fraction of the acute mortality from CO is due to hypoxia, however, and prompt removal of CO from hemoglobin will be of benefit . HBO2 also promotes normalization of tissue hypoxia. CO binds to cytochrome oxidase, particularly when the COHb level exceeds 40% to 50% . Brown and Piantadosi demonstrated that hyperbaric oxygen at 3 ATA markedly accelerates the dissociation of CO from cytochrome oxidase. Furthermore, it was shown that HBO2 completely reversed brain mitochondrial electron transport chain inhibition by CO. Hyperbaric oxygen also has effects related to the cascade of vascular injury triggered by CO poisoning. Hyperbaric oxygen was found to be effective for preventing brain oxidative injury through increased heme oxygenase and upregulation of antioxidants. The mechanism appears to be associated with denaturation of a membrane-associated guanylate cyclase that plays a role in coordinating the elevated affinity of beta 2 integrins expressed on the cell surface. Given that vascular changes are prominent in clinical CO poisoning, it is feasible that neurological sequelae in patients may involve a perivascular injury mediated by leukocyte sequestration and activation. Moreover, HBO2 reduces neuronal apoptosis and necrosis, and it also mobilizes stem cells via a nitric oxide–dependent mechanism. Hence, timely administration of hyperbaric oxygen may ameliorate the cascade leading to brain injury via multiple mechanisms.